Respond to an Overdose
When someone stops breathing, every second matters. Knowing what to do, calling 9-1-1 and using naloxone can prevent an accidental opioid overdose from becoming deadly. And the data show that all these efforts are making a difference. Community members like you are reversing around 20% of the reported non-fatal overdoses. You are saving the lives of your family members, friends and neighbors.
Signs and symptoms of an opioid overdose include:
- Blue/purple fingernails or lips
- Pale face
- Stopped breathing, slow breathing or heartbeat
- Gasping, gurgling or loud snoring sounds
- Vomiting
- Inability to speak or stay awakened
- Limp body
- Unresponsive to yelling or touch
Brief video by Bangor Public Health & Community Services to explain the signs of overdose and how to save a life.
If you think someone is experiencing an opioid overdose, follow these emergency steps:
- See if they are responsive
- Call the person’s name.
- If this doesn’t work, vigorously rub your knuckles on the person’s sternum (the breastbone in the middle of the chest) or rub knuckles on the person’s upper lip.
- If the person is not breathing normally and/or talking, call 9-1-1 and continue to check them.
- DON’T use a cold shower or ice to shock someone. This increases the risk of falling, drowning, or going into shock.
- Call 9-1-1
- IMMEDIATELY seek medical attention by calling 9-1-1. Tell the operator: “Someone is unresponsive and not breathing.”
- Be sure to give a specific address and/or a description of your location.
- Give naloxone
- For a 30-second explanation of how to use nasal naloxone, watch this video from CDC: https://www.youtube.com/watch?v=odlFtGNjmMQ&t=1s
- For an explanation of how to use injectable naloxone, watch this video.
- Wait 2 to 3 minutes after giving the first dose of naloxone. If the person does not respond, give a second dose.
- Always give naloxone–even if you are uncertain the person used opioids. Naloxone will have no negative effects if given when it is not needed.
- Help the person breathe
- Start rescue breathing by doing CPR while you wait for the ambulance.
- Follow these steps:
- Place the person on their back and give 30 chest compressions (approximately 18 seconds).
- Hand position: Two hands centered on the chest
- Body position: Shoulders directly over hands; elbows locked
- Depth: At least 2 inches
- Rate: 100 to 120 per minute
- Allow chest to return to normal position after each compression
- Check the person’s mouth and throat to make sure nothing is blocking the airway.
- Place one hand on the person’s chin, tilt the head back, and pinch the nose closed.
- Place your mouth over the person’s mouth to make a seal, give two slow breaths (1 second each), and watch for the person’s chest to rise.
- Continue giving sets of 30 compressions and 2 breaths. Use an AED (automated external defibrillator) if available.
- Place the person on their back and give 30 chest compressions (approximately 18 seconds).
- Follow these steps:
- Start rescue breathing by doing CPR while you wait for the ambulance.
- Monitor the person’s response
- Stay with the person and keep them warm.
- Watch for signs of the overdose returning for at least 4 hours from the last dose of naloxone. Naloxone is short-acting, and opioids may remain in the body for longer.
- Get medical care as quickly as possible, even if the person revives after receiving naloxone and seems to feel better, as overdose symptoms may return.
- Put the person in the “recovery position” (on their side, with the top leg bent and one arm under their head–see below). This will help prevent them from choking.

Learn How to Use Naloxone
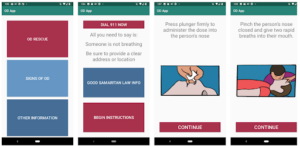
Get the OD-ME mobile app for step-by-step audio instructions to follow during the stress of an overdose (screenshots below). Learn more about naloxone or download our Naloxone FAQ sheet.